Why Timing Matters for Your Medical Device Startups
Introduction
The medical device industry is evolving rapidly, and regulatory compliance is becoming increasingly stringent. While most medical device startups understand what they need to do, few focus on when to do it.
Under the Medical Device Regulation (MDR), the timing of your clinical strategy is just as critical as the strategy itself. Properly timed clinical evidence collection can streamline regulatory approval, reduce costs, and accelerate market entry. On the other hand, poor timing can result in compliance delays, regulatory rejections, and significant financial setbacks.
So, how can startups optimize their clinical strategy to align with MDR? This guide breaks down the essential timing considerations and best practices to avoid unnecessary roadblocks.
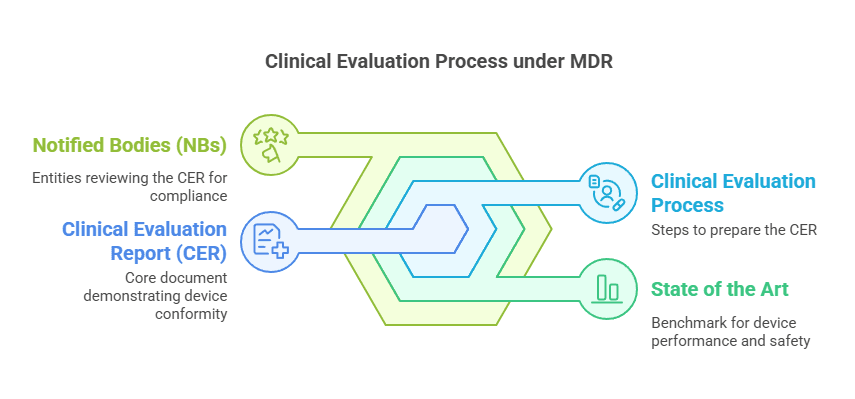
Understanding Clinical Strategy Under MDR
A successful clinical strategy for medical device approval must be structured and time-sensitive. It should include:
- Regulatory Pathway – Identify the applicable clinical evaluation process (Article 61, MDR).
- Clinical Evidence Requirements – Determine the type and adequacy of clinical data (Annex XIV, MDR).
- Pre-Market & Post-Market Clinical Planning – Implement continuous Post-Market Clinical Follow-up (PMCF) strategies (Annex XIV Part B, MDR).
Why It Matters
- A well-defined clinical strategy aligns with MDR requirements, ensuring a smoother approval process.
- Delays in evidence collection can extend approval timelines and increase compliance costs.
How Poor Timing Can Delay Medical Device Approval
One of the most common pitfalls startups face is underestimating the role of timing in regulatory approval. Poor clinical strategy planning can lead to:
- Regulatory Non-Compliance – Insufficient or untimely clinical data may delay or prevent certification.
- Extended Market Entry Timelines – A lack of early planning adds months or even years to device approval.
- Increased Financial Strain – Correcting regulatory errors late in the process results in higher costs.

Case Study: The Cost of Late Clinical Planning
A Class IIb medical device startup initially focused only on product development, neglecting early regulatory engagement. This oversight resulted in:
- A nine-month approval delay due to missing pre-market clinical data.
- Over €300,000 in additional compliance costs for new clinical trials.
- Lost market opportunity as competitors launched similar devices first.
This example highlights the importance of early clinical planning and regulatory engagement in achieving faster approvals.
Best Practices for Timing Your Clinical Strategy
1) Engage Early with Notified Bodies
- Contact Notified Bodies (NBs) early to understand clinical evidence expectations.
- Seek regulatory guidance before starting clinical investigations.
2) Align Clinical Evidence Collection with MDR Phases
- Pre-market clinical studies should be planned well in advance.
- Post-Market Clinical Follow-up (PMCF) should be incorporated into the long-term strategy.
3) Maintain Compliance with State of the Art Literature Searches
- Regularly update literature search data to support device safety claims.
- Ensure alignment with current medical and scientific standards.
4) Adopt a Risk-Based Approach
- Tailor your clinical evidence plan based on device classification and intended use.
- Higher-risk devices require more extensive clinical investigations.
A structured and time-sensitive approach ensures faster approvals, lower costs, and better market positioning.
Frequently Asked Questions (FAQ)
1) How does timing affect MDR approval for medical devices?
Timing is critical because MDR requires structured clinical evidence collection at specific stages. If key milestones are missed, regulatory bodies may reject the submission or request additional data, leading to delays.
2) When should a medical device startup start engaging with a Notified Body?
It’s best to engage early, preferably before clinical trials begin. Frequent communication ensures that the clinical evidence plan meets MDR requirements.
3) What happens if a startup delays clinical strategy planning?
Delayed planning can result in:
- Regulatory rejections due to incomplete clinical data.
- Extended approval timelines as additional clinical trials are required.
- Increased costs from compliance corrections and re-submissions.
4) How can medical device startups optimize their clinical strategy for MDR?
Startups should:
- Plan pre-market and post-market clinical evaluations early.
- Use systematic literature searches to meet MDR requirements.
- Engage regulatory experts and Notified Bodies proactively.
- Follow MDCG guidance to stay compliant.
5) What are the key requirements for PMCF under MDR?
Post-Market Clinical Follow-up (PMCF, Annex XIV, MDR) ensures that clinical evidence is continuously updated after a device is on the market. Failure to implement PMCF can lead to compliance violations and potential market withdrawal.
Final Thought: Timing is Everything
For medical device startups, timing is a strategic advantage. Poor planning leads to compliance risks, extended timelines, and financial strain.
What challenges have you faced in aligning your clinical strategy with MDR? Share your insights below.
If this was helpful, share it with someone in your network who might need it.
PS: For more information, subscribe to my newsletter and get access to exclusive content, private insights, and expert guidance on MDR compliance and CE marking: Subscribe Here
✌️ Peace,
Hatem Rabeh, MD, MSc Ing
Your Clinical Evaluation Expert & Partner
Contact me for more insights and practical advice!