Why Vigilance Reporting for CE-Marked Devices Still Matters During Clinical Investigations
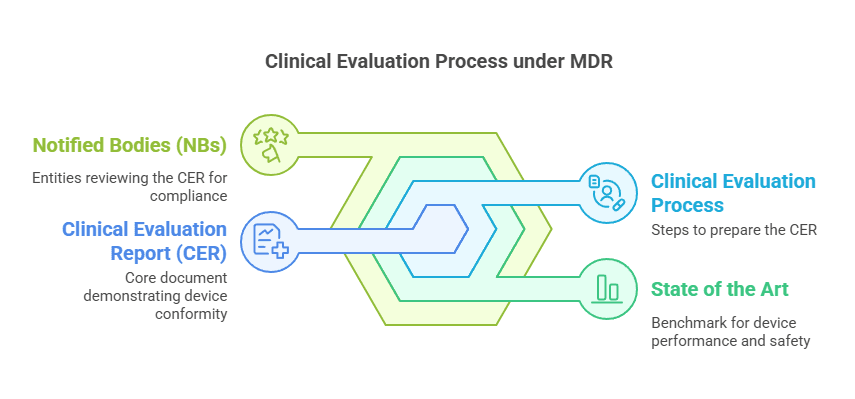
The MDCG 2023-3 Rev.2 guidance document contains a flowchart that explains how vigilance integrates into the broader regulatory framework.
Even the most experienced regulatory affairs engineers ask this question—“If a CE-marked device is used in a clinical investigation, does the manufacturer still need to report serious incidents?” It’s a fair question. After all, a CE mark often signals regulatory compliance, safety, and readiness for market. So why does vigilance still apply?
Well, let’s clear that up. The short answer? Yes, it absolutely still applies.
CE Mark Does Not Mean “Vigilance Exempt”
CE marking is a powerful symbol, no doubt. It tells the world that your medical device meets all applicable European requirements. But here’s the catch: a CE mark doesn’t grant immunity from vigilance obligations—especially not when that device is part of a clinical investigation, a PMCF study, or being used in a real-world setting for its intended purpose.
In fact, according to MDR Article 87(1) and MDCG 2023-3 Rev.2, the obligations are clear: serious incidents involving a CE-marked device must be reported, regardless of the setting.
Breaking It Down: The Legal Framework
Let’s demystify what MDR Article 87(1) actually says. It outlines the mandatory vigilance reporting process for manufacturers, requiring:
Timely reporting of serious incidents
Trend reporting for non-serious incidents
Corrective actions to mitigate future risk
And this applies even if the device is already CE-marked and undergoing a clinical investigation.
Here’s why:
Clinical investigations aren’t “testing phases” exempt from regulation.
Once a device is out in the field—whether through a PMCF study, clinical trial, or standard use—it’s interacting with real human lives. Therefore, vigilance remains critical.Data integrity depends on it.
Missing a vigilance report can delay your Clinical Evaluation Report (CER), your PSUR, or even worse—get you flagged by a Notified Body or Competent Authority.
Clinical Scenario: A Hard Lesson Learned
I’ve personally seen a regulatory team delay their CER submission by several months due to a missed vigilance report during a PMCF study. They assumed the CE mark meant fewer reporting obligations.
Big mistake.
And unfortunately, I’ve also seen Competent Authorities reject PSURs for the same reason. It’s a painful, preventable error that costs teams time, money, and credibility.
Best Practices to Avoid This Pitfall
Let’s not just dwell on what could go wrong. Here’s how to get it right:
✅ Build Vigilance into Your Clinical Strategy Early
Incorporate vigilance reporting into your study planning. Make sure your clinical and RA teams are aligned before the study begins.
✅ Train Your Teams on Reporting Requirements
Everyone involved—CROs, clinical teams, even your post-market surveillance colleagues—must know when and how to report.
✅ Use the MDCG 2023-3 Rev.2 Flowchart
This document is gold. It visually explains how vigilance fits into the broader regulatory framework. Post it on your office wall, embed it into SOPs, or attach it to your training slides.

What About PMCF Studies?
Here’s a common follow-up: “If the study is post-market, do the same rules apply?”
Absolutely. PMCF doesn’t change vigilance obligations. Whether it’s a registry, a case series, or a usability study, serious incidents must still be reported. Don’t let the “post-market” label trick you into complacency.
The Bottom Line on Vigilance Reporting for CE-Marked Devices
Regulatory compliance doesn’t stop with a CE mark. In fact, it might just be getting started.
Whether your device is in a pre-market clinical investigation, post-market study, or regular clinical use, vigilance is non-negotiable. Build your systems, train your people, and always, always report.
Because vigilance isn’t just about compliance—it’s about patient safety.
FAQs
Is vigilance reporting required during a clinical investigation of a CE-marked device?
Yes. According to MDR Article 87(1), serious incidents must be reported even during clinical investigations involving CE-marked devices.
What if the device is being used for its intended purpose in a real-world setting?
Vigilance obligations still apply. Intended use does not exempt the manufacturer from reporting.
Can missing a vigilance report delay my CER?
Absolutely. I’ve seen CER timelines stretch by months due to missed incident reporting during clinical trials.
Do post-market studies (PMCF) change vigilance obligations?
No. PMCF studies are still part of the post-market lifecycle, and vigilance reporting is mandatory.
Where can I find guidance on how vigilance fits into MDR requirements?
The MDCG 2023-3 Rev.2 guidance document contains a flowchart that explains how vigilance integrates into the broader regulatory framework.
What are the penalties for non-compliance?
Non-compliance can result in regulatory findings, delayed approvals, and potential product withdrawals from the market.
Final Thoughts
When it comes to clinical investigations, don’t let the CE mark lull your team into a false sense of security. Vigilance doesn’t pause when a study starts—it becomes even more critical. Whether your device is in a PMCF study, a real-world setting, or an early-stage clinical trial, your obligation to report serious incidents remains unchanged.
In fact, this is where regulatory discipline and clinical excellence intersect. Missed vigilance signals during a study don’t just jeopardize your CER or PSUR—they compromise the trust regulators place in your processes.
So here’s my advice, from one medical device professional to another:
Make vigilance a part of your clinical DNA.
Educate your teams before the first patient is enrolled.
Build reporting pathways that work in real time—not just in theory.
Because at the end of the day, good vigilance isn’t just about compliance. It’s about building better, safer medical devices—devices that stand up to scrutiny, perform under pressure, and ultimately, improve lives.
PS: For more information, subscribe to my newsletter and get access to exclusive content, private insights, and expert guidance on MDR compliance and CE marking: Subscribe Here
✌️ Peace,
Hatem Rabeh, MD, MSc Ing
Your Clinical Evaluation Expert & Partner
Follow me for more insights and practical advice!