Proven Strategies to Define Performance Objectives for Medical Devices That Meet EU MDR Standards
The Crucial Role of Performance Objectives in Medical Device Compliance
When it comes to medical device development, precision is everything. That’s especially true under the stringent lens of the European Union Medical Device Regulation (EU MDR). Among its numerous requirements, one stands out as both foundational and strategic: performance objectives.
As a clinical evaluation specialist and practicing medical doctor, I’ve seen firsthand how clearly defined performance objectives can shape a device’s success—both in terms of patient outcomes and regulatory compliance. These aren’t just metrics; they are proof points. They demonstrate your device’s ability to safely deliver on its intended purpose while maintaining alignment with the state of the art (SOTA).
But what exactly are these objectives? Why do they matter so much? And most importantly, how can you build them to satisfy both regulators and clinicians?
Let’s dive into this critical element of medical device development and unravel how to get it right.
What Are Performance Objectives in Medical Devices?
In simple terms, performance objectives are specific, quantifiable goals that a medical device must meet to be considered safe and effective. They act as guiding metrics throughout the device lifecycle—spanning pre-clinical development, clinical evaluation, and post-market surveillance.
For instance, in a continuous glucose monitor, a performance objective could be:
“Maintain blood glucose readings within the range of 70–180 mg/dL for at least 85% of monitoring time.”
These objectives give manufacturers a concrete target, allowing clinical teams to measure whether a device achieves its clinical benefits without imposing undue risk.
Why EU MDR Compliance Starts with Performance Objectives
EU MDR mandates that medical devices demonstrate safety and performance through structured and scientifically validated processes. According to Annex XIV Part A, performance objectives must align with:
The intended purpose of the device
The current state of the art
Comparable benchmarks, if available
Clinical benefits and risk profiles
This is not optional. Regulatory bodies expect manufacturers to define, measure, and defend their performance goals throughout the clinical evaluation process.
When manufacturers establish clear and relevant objectives early, they can avoid unnecessary roadblocks during conformity assessment. It’s the difference between a smooth submission and a prolonged approval cycle.
Clinical Perspective on Setting Objectives That Matter
Let’s face it: too many clinical evaluations fall into the trap of generality. Vague goals like “improve patient comfort” don’t cut it.
From a clinical standpoint, performance objectives should answer three questions:
What exactly are we trying to improve or measure?
How does this improvement reflect real-world usage or patient benefit?
Is there credible, comparative data supporting this claim?
For example, a device intended to reduce post-operative bleeding must have specific endpoints such as “Reduce average post-surgical blood loss by ≥30% compared to standard care.” Vague claims fail to satisfy regulators—and don’t help patients either.
Essential Elements Every Performance Objective Must Include
To be regulatory-ready and scientifically robust, every performance objective should include:
A clearly defined outcome measure (e.g., HbA1c reduction, wound healing time)
Numerical thresholds or targets (e.g., ≥90% success rate)
Time frames (e.g., within 7 days post-operation)
Comparative reference points (e.g., literature data, predicate devices)
Think of it as a SMART goal for your clinical evaluation.
Connecting Performance Objectives to the Device’s Purpose
A well-constructed objective is one that tightly reflects the device’s intended use. If a device is designed for cardiac arrhythmia detection, the objective should not drift into general cardiovascular wellness.
Instead, anchor the goal. For example:
“Detect ≥95% of clinically significant atrial fibrillation episodes within 24 hours of onset.”
This not only sharpens the claim but gives regulatory reviewers a transparent benchmark to assess.
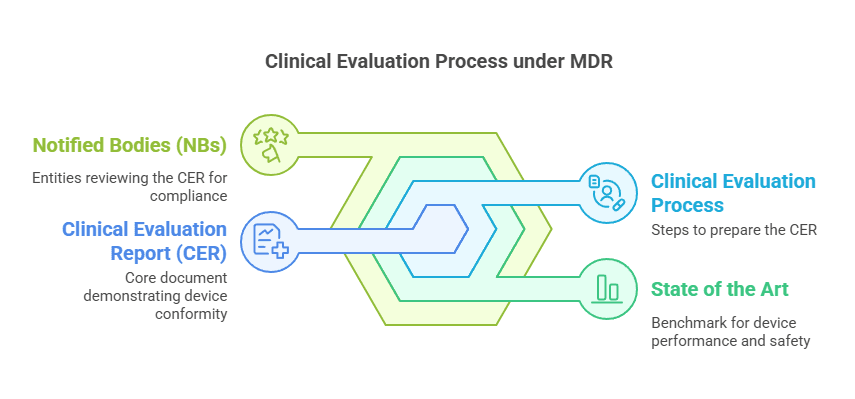
Understanding Article 61 and Annex XIV of the EU MDR
Article 61 and Annex XIV of EU MDR provide the blueprint for clinical evaluations. They emphasize that manufacturers must justify performance objectives in light of:
Risk-benefit ratio
SOTA comparisons
Clinical data sources (including literature and post-market data)
So, don’t just pick a number. Provide scientific rationale—especially when claiming superiority or innovation.
How to Align Performance Objectives with the Current SOTA
SOTA isn’t just a buzzword—it’s the standard you must match or exceed.
To align with it:
Conduct systematic literature reviews of current treatments and devices.
Identify benchmark devices with proven outcomes.
Incorporate recent clinical guidelines (e.g., from ESC, NICE, FDA, etc.).
Let’s say an implantable defibrillator claims a 99% shock accuracy rate. That becomes your minimum performance threshold—unless you have data proving a higher standard.
Using Systematic Literature Reviews to Benchmark Performance
Systematic reviews are gold when defining performance metrics. Here’s a simple method:
Define inclusion/exclusion criteria for comparable devices.
Extract reported performance rates (e.g., sensitivity, specificity, adverse event rates).
Summarize data in a performance matrix.
This exercise ensures that your objectives are anchored in evidence, not assumption.
Leveraging Clinical Practice Standards in Performance Targeting
Aligning with established clinical guidelines like those from WHO, ECDC, or medical societies boosts your credibility.
For instance, if NICE recommends an infection control threshold of ≤5% post-procedure, and your device promises ≤2%, that’s a strong, defensible objective.
Top Methodologies for Setting Measurable Performance Goals
Here are proven methodologies:
Comparative Analysis: Use real-world or published data to match benchmarks.
Delphi Panels: Gain consensus from expert clinicians.
Bayesian Modeling: Ideal for early-stage or niche devices.
GHTF and IMDRF Frameworks: Apply globally accepted methods.
Every methodology must be justifiable, reproducible, and relevant.
Benchmarking Against Existing Devices for Competitive Edge
If your competitor’s device achieves 92% sensitivity in cancer detection, yours must aim for at least the same—preferably higher, or with fewer side effects.
Use comparative tables to position your device:
| Parameter | Benchmark Device | Your Device |
|---|---|---|
| Detection Accuracy | 92% | 95% |
| Time to Result | 2 hours | 1 hour |
| False Positives | 6% | 3% |
Such data convinces not just regulators—but clinicians and payers, too.
Examples of Objective Metrics: From Blood Glucose to Efficacy Rates
Let’s look at real-world performance objectives:
Diabetes Monitor: ≥85% time in range (70–180 mg/dL) over 7 days
Wound Dressing: ≥95% healing within 14 days
Diagnostic Kit: Sensitivity ≥98%, Specificity ≥99%
Surgical Robot: Accuracy deviation ≤1.5 mm
Define. Quantify. Deliver.
Balancing Risk and Performance Expectations
Performance objectives must reflect a balanced risk-benefit ratio. If you’re promising higher accuracy, are you also increasing adverse event risks?
Use ISO 14971-based risk analysis to align expectations.
Best Practices for Performance Documentation in CEP
Your Clinical Evaluation Plan (CEP) must clearly articulate:
Objective statements
Supporting evidence
Methods of measurement
Rationale for thresholds
Use visual aids and flow diagrams to enhance clarity.
Post-Market Surveillance and Ongoing Validation
Even after launch, performance objectives are not set in stone. Post-market surveillance (PMS) may reveal new risks or usage patterns that require objective recalibration.
Make PMS a feedback loop for continuous improvement.
Stakeholder Involvement in Performance Validation
Engage early and often with:
Clinicians
Biomedical engineers
Regulatory consultants
Patients (especially for usability metrics)
Their insights make your objectives both clinically relevant and operationally feasible.
FAQs
How are performance objectives different from clinical endpoints?
Objectives guide development and evaluation, while endpoints are specific outcomes used in trials.
Can performance objectives be qualitative?
They should be quantifiable. Even qualitative aspects can be translated into measurable indicators.
What if my device has no direct comparator?
Use literature, expert panels, or analogous devices to derive realistic thresholds.
How often should performance objectives be updated?
They should be reviewed annually and after major updates, recalls, or new PMS data.
Are performance objectives necessary for Class I devices?
Yes, though the depth and specificity may vary based on the device’s risk profile.
Is there a template for documenting performance objectives?
Most companies use a custom template, but it must align with Annex XIV and be referenced in the CEP.
Final Thoughts
Defining performance objectives is as much a science as it is a strategy. When approached thoughtfully, they help you achieve:
Smoother regulatory reviews
Stronger clinical outcomes
Greater trust with stakeholders
PS: For more information, subscribe to my newsletter and get access to exclusive content, private insights, and expert guidance on MDR compliance and CE marking: Subscribe Here
✌️ Peace,
Hatem Rabeh, MD, MSc Ing
Your Clinical Evaluation Expert & Partner
Follow me for more insights and practical advice!