How Often Should You Really Update a Clinical Evaluation Report (CER)?
Clinical Evaluation Reports (CERs) are the regulatory backbone of medical devices in Europe. Yet, from working hands-on with teams across the industry, one persistent problem keeps cropping up—delayed updates. The document might be submitted once, checked off, then forgotten… until an audit unearths non-conformities that could’ve been avoided.
In this guide, we’ll answer the essential question: How often should you update your Clinical Evaluation Report? Along the way, you’ll gain clarity from MEDDEV 2.7/1 Rev. 4, audit experiences, and real-world practices that help medical device manufacturers stay compliant—and sane.
Why Update a Clinical Evaluation Report (CER)?
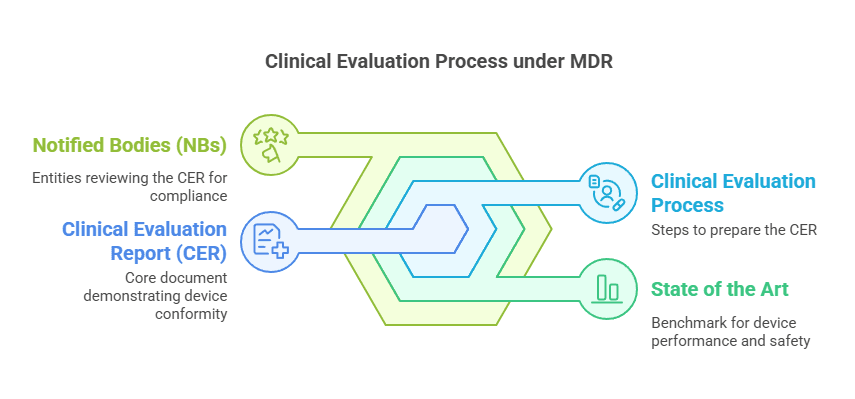
Updating your CER isn’t just a compliance checkbox—it’s an ongoing, dynamic obligation. Notified bodies expect your CER to reflect the current state of knowledge, real-world performance, and evolving safety profiles. It’s part of a continuous clinical evaluation process, not a one-time effort.
Neglecting updates can result in serious consequences, like:
Major non-conformities during audits
Certification delays or suspensions
Regulatory warning letters
Increased scrutiny during technical documentation assessments
Staying current is not optional—it’s a strategic imperative.
What MEDDEV 2.7/1 Rev. 4 Says About CER Update Frequency
Let’s break it down based on Section 6.2.3 of MEDDEV 2.7/1 Rev. 4.
Annual Updates Required For:
Class III devices
Class IIb implantable devices
Devices not well established on the market
These are considered higher risk or lacking sufficient long-term data. Hence, regulators expect annual reviews to ensure conclusions remain valid.
Updates Every 2 to 5 Years Could Be Justified For:
Low-risk, well-established devices
However, this leniency comes with strings attached. The manufacturer must provide a clear, evidence-based justification. This rationale should be documented in the Quality Management System (QMS) and referenced within the CER itself.
Immediate Updates Are Mandated When:
New PMS (Post-Market Surveillance) data
New PMCF (Post-Market Clinical Follow-up) results
Emerging safety signals or adverse events
Device design or IFU changes
These events can shift the clinical benefit-risk profile and therefore must be addressed without delay.
The Regulatory and Strategic Case for Updating CERs Regularly
Failing to update your CER is like navigating with an outdated map. It not only risks regulatory trouble but can obscure important safety insights that should inform future product development and clinical strategies.
CERs Are Living Documents
Treating the CER as a static file is a mistake—regulatory bodies expect a living, breathing document that evolves with the product and its real-world use.
Clinical Evaluation and PMS/PMCF: A Synchronized Strategy
One of the most effective ways to streamline CER updates is to align them with PMS and PMCF cycles.
Example: If you conduct PMCF studies annually or every two years, schedule your CER updates to coincide with those milestones.
Why it works: You minimize duplicated efforts, capture data while it’s fresh, and keep the report up-to-date by default.
What I Recommend as a Clinical Evaluation Consultant
Having reviewed dozens of CERs over 8+ years, from Class I disposables to implantable Class III systems, I’ve developed a few key strategies that consistently help teams succeed.
✅ Align With Real-World Data Cycles
Whether it’s PMCF, literature reviews, or vigilance tracking—link your update schedule to when new data becomes available.
✅ Set Expectations in Your QMS
Document your rationale for update frequency. Whether it’s annual or every 3–5 years, be ready to defend it. This small step builds confidence during audits.
✅ Use Literature and Vigilance as Triggers
New studies? Adverse event trends? Literature that contradicts your clinical claims? Each is a signal to review your CER—even if your next scheduled update isn’t due.
Documented Justification: The Secret Weapon in Audit Defense
One of the most overlooked yet powerful tools is a written justification for your CER update frequency. Add this to your QMS, your CER, and ideally to your Risk Management File (RMF).
Is your device low risk?
Have there been zero significant safety signals?
Is your clinical state of the art unchanged?
Then say so clearly, and back it up with real data. This transparency can satisfy even the toughest notified body auditors.
Why “More Data” Isn’t Always the Answer
Contrary to popular belief, many teams don’t fail audits because they lack data—they fail because they haven’t organized or interpreted the data correctly.
No PMS trending?
No updated literature review?
No linkage between PMCF and clinical conclusions?
That’s where the real problems start. Data without context can’t save your CER from scrutiny.
Lessons From the Field: What Notified Bodies Look For
Auditors don’t just skim your CER. They often triangulate it against your PMS reports, Risk Management File, and PMCF plans. Any mismatch can raise red flags.
For instance:
If your CER says “no safety issues,” but your PMS has a spike in complaints—that’s a problem.
If your last literature review is over 3 years old, they’ll ask: “Why?”
If your PMCF plan hasn’t been executed, they’ll say the CER lacks evidence.
How Often Should You Update a Clinical Evaluation Report (CER)?
Let’s answer the question clearly.
Update your CER:
Annually, if your device is Class III, IIb implantable, or not well-established
Every 2–5 years, only if your device is low-risk, well-established, and your justification is rock solid
Immediately, if PMS or PMCF data changes your conclusions
More importantly, tie CER updates to real-world events—not just the calendar.
FAQs About Updating Clinical Evaluation Reports
How often should I update my CER for a Class IIa device?
If the device is well-established with a long safety history, updating every 2–3 years may be acceptable—with documented justification.
Can I justify not updating my CER annually?
Yes, but only for low-risk, well-established devices and only if the rationale is documented and based on evidence.
Do I need to update the CER if no new PMS data is available?
Yes. Lack of data should still be analyzed, and a justification for non-update must be included in the CER.
Should my CER and PMS report be written together?
Ideally, yes. Synchronizing these documents ensures consistency and saves time during audits.
What if my notified body disagrees with my update frequency?
You must be able to defend your position with structured reasoning and supporting evidence. If in doubt, update more frequently.
Is a five-year CER update ever acceptable?
Rarely. Only in exceptional cases where risk is minimal, performance is proven, and there are no new findings.
Final Thoughts
Instead of thinking of the CER as a “compliance document,” consider it a clinical intelligence tool. It should guide product decisions, support your market strategy, and reflect your commitment to patient safety and performance excellence.
Update early, update smart, and you’ll avoid audit panic, regulatory delays, and most importantly—risk to patients.
PS: For more information, subscribe to my newsletter and get access to exclusive content, private insights, and expert guidance on MDR compliance and CE marking: Subscribe Here
✌️ Peace,
Hatem Rabeh, MD, MSc Ing
Your Clinical Evaluation Expert & Partner
Follow me for more insights and practical advice!