Clinical Investigation Pathways for CE-Marked Medical Devices
Conducting clinical investigations on CE-marked medical devices within the European regulatory framework is no small feat. It demands deep scientific understanding and strategic regulatory planning.
With the introduction of the Medical Device Regulation (EU) 2017/745 (MDR) and MDCG 2021-6 Rev.1 guidance, sponsors and manufacturers must now to go throught a more nuanced landscape.
This article sheds light on the regulatory routes available for CE-marked medical devices during clinical investigations, particularly for post-market and conformity assessment purposes.
Let’s break down these pathways clearly and effectively.
Regulatory Pathways for CE-Marked Devices
Clinical investigations under the MDR fall into structured categories based on device status and usage. For CE-marked devices, the first regulatory crossroad involves determining whether the device will be used within its intended purpose.
Understanding Intended Purpose
The concept of “intended purpose” is foundational to determining regulatory compliance. As outlined in the device’s instructions for use (IFU), this includes:
Clinical indications
Contraindications
Target patient group(s)
Expected users (e.g., clinician, patient)
If the investigation proposes a deviation from this established scope, it triggers a different regulatory pathway—potentially moving from post-market clinical follow-up (PMCF) to a full conformity assessment.
What Qualifies as a Clinical Investigation?
Per MDR Article 2(45), a clinical investigation is defined as a systematic investigation involving human subjects aimed at assessing safety and performance of a device. It’s vital to differentiate this from broader clinical research or “clinical studies,” a term encompassing:
Medicinal product trials
Device investigations
In vitro diagnostics (IVD) studies
Not all device-related research is a clinical investigation. Thus, sponsors must evaluate their study design early to determine the applicable route.
Three Core Regulatory Pathways
The MDR provides three main regulatory channels, depending on the nature of the device and its use:
Article 62: For devices not yet CE-marked or being used outside their intended purpose.
Article 74(1): For CE-marked devices used within their intended purpose, typically as part of PMCF.
Article 82: For non-conformity-related investigations, often driven by scientific or health policy objectives and subject to national laws.
Each path has unique documentation, notification, and timing requirements, affecting project timelines and stakeholder involvement.
Delving Into Article 74(1): PMCF Investigations
PMCF activities ensure continued evaluation of device safety and performance after CE marking. However, if these investigations introduce invasive or burdensome procedures, sponsors must notify competent authorities.
When Is a Procedure Considered Invasive or Burdensome?
Examples include:
Additional imaging (e.g., MRI, CT scans)
Biopsy or extra blood draws
Prolonged procedural durations
Additional follow-ups outside normal practice
Notably, MDCG 2021-6 Rev.1, Question 11, is the key reference here. Misjudging this distinction can result in regulatory non-compliance or delayed study starts.
Documentation Checklist for Article 74(1) with Additional Procedures
If the study includes invasive/burdensome interventions, you must:
Notify each Member State at least 30 days before initiation
Submit documents outlined in Annex XV, Chapter II of the MDR
Use the electronic system described in Article 73
This includes:
Clinical Investigation Plan (CIP)
Investigator’s Brochure (IB)
Subject Information Sheet (SIS)
Informed Consent Form (ICF)
When to Choose Article 62
If you’re evaluating a CE-marked device outside its declared purpose, your investigation will likely fall under Article 62. In this case:
A formal application must be submitted for review and approval
A clinical investigation application dossier must be compiled, as outlined in Annex XV
Ethics committee approval is mandatory
This route often involves more scrutiny and longer lead times.
Understanding Article 82 Investigations
Article 82 covers non-conformity-related investigations that don’t fit within Articles 62 or 74. These are often:
Investigator-initiated trials
Public health-driven assessments
Academic research
Here, national legislation plays a critical role, and approval procedures may differ widely across EU Member States.
Use of MDCG 2021-6 Rev.1 Flowchart
Annex I of MDCG 2021-6 Rev.1 provides a valuable decision-tree flowchart to identify the correct regulatory pathway. To use this tool:
Confirm CE marking status
Determine if the device is used within intended purpose
Identify if additional procedures are invasive or burdensome
Establish conformity objectives
This visual guide supports consistent and accurate regulatory planning.

National Requirements: One Regulation, Many Interpretations
While MDR is harmonized EU law, its application can differ per Member State. For instance:
Germany (BfArM) may require separate ethics and authority submissions
France (ANSM) mandates additional data protection compliance
UK (MHRA), post-Brexit, operates under UK MDR and IRAS for submission, requiring 60-day notification
Regulatory Strategy and Quality Integration
All clinical investigations should be governed under your Quality Management System (QMS). This ensures:
Document control for audit readiness
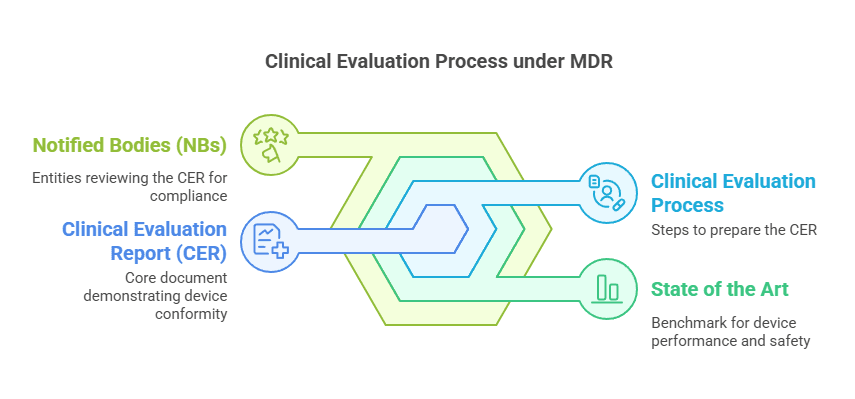
Integration with Clinical Evaluation Reports (CER)
Linkage to risk management and PMS
ISO 14155:2020 compliance is critical for global acceptance and regulatory scrutiny.
Best Practices for Sponsors
To successfully navigate the regulatory environment:
Start early with regulatory pathway assessment
Maintain up-to-date documentation
Engage with competent authorities proactively
Leverage expert consultations where national requirements are ambiguous
FAQs
Is ethics approval needed for Article 74(1) PMCF studies?
Yes, especially if the investigation includes additional burdensome procedures or deviates from standard care.
Can we submit the same dossier for multiple Member States?
Yes, but be prepared to address national variations in application content and formatting.
What if I’m unsure about procedure classification?
Consult with the relevant national competent authority early in the process.
Do all CE-marked device investigations require notification?
Only if they involve burdensome or invasive procedures beyond the intended use.
How soon can we start the investigation after notification?
For Article 74(1), there’s typically a 30-day waiting period post-notification unless extended by the authority.
What if our study spans multiple EU countries?
Expect variations in ethical review timelines, submission platforms, and documentation needs.
Final Thoughts
Successfully conducting clinical investigations with CE-marked devices under the MDR requires a detailed understanding of the regulatory pathways, device intent, and procedural burden. The MDCG 2021-6 Rev.1 guidance, especially Annex I and Question 12, remains the cornerstone reference for such studies.
Sponsors must integrate clinical investigations into their broader QMS, plan for national variations, and prioritize early regulatory engagement to streamline approvals. By doing so, you not only ensure compliance but also contribute to a robust evidence base that supports patient safety and device efficacy.
PS: For more information, subscribe to my newsletter and get access to exclusive content, private insights, and expert guidance on MDR compliance and CE marking: Subscribe Here
✌️ Peace,
Hatem Rabeh, MD, MSc Ing
Your Clinical Evaluation Expert & Partner
Follow me for more insights and practical advice!